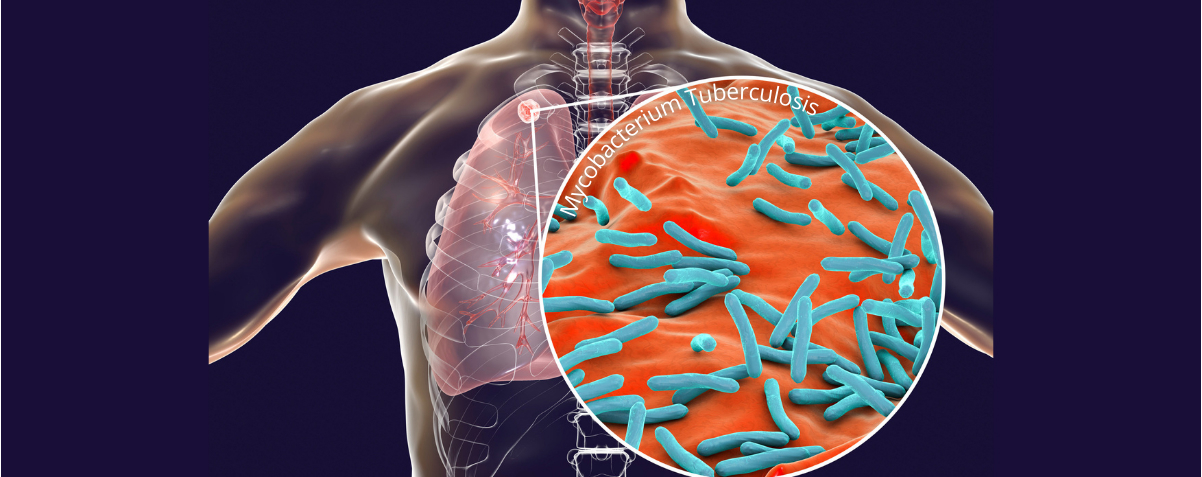
While COVID-19, a disease caused by a virus, has captured the world’s attention over the past year, bacterial infections continue unabated. Furthermore, the emergence of more and more “superbugs” that are resistant to current treatment only serves to compound the issue, often leading to deadly outcomes. The Mycobacterium tuberculosis (Mtb) bacteria that causes tuberculosis (TB) is one of those superbugs.
Like COVID-19, TB is an easily transmissible airborne disease. It has plagued humans for thousands of years and continues to be one of the top ten causes of death worldwide today. The problem has worsened with the emergence of Mtb strains that have developed resistance to available treatments, giving rise to drug-resistant tuberculosis (DR-TB). In 2019, the World Health Organisation assessed that approximately 10 million people worldwide were infected with TB – among whom 500,000 developed DR-TB, and 182,000 died.
As a result, research to uncover the inner mechanisms of the Mtb bacterium has been ongoing in order to combat DR-TB and develop novel drugs to tackle this intractable disease. Scientists from the Experimental Drug Development Centre (EDDC), the national platform for drug discovery and development hosted by Agency for Science, Technology and Research (A*STAR), Nanyang Technological University (NTU) and Lee Kong Chian School of Medicine (LKC Medicine) have teamed up to develop two classes of potential drug candidates against DR-TB.
The Mtb bacteria generates the energy it needs to live and reproduce through a process known as oxidative phosphorylation. This pathway is a series of biological and chemical reactions that use key proteins (enzymes) to catalyse the formation of “energy carrying” molecules called ATP (adenosine triphosphate). ATP is what powers the bacterium to live and reproduce. Disrupting or inhibiting this pathway would therefore kill the bacteria.
“The enzymes in the oxidative phosphorylation pathway of Mtb have epitopes – unique regions that are specific to the bacteria – which are attractive targets for the design of drugs that inhibit or kill the pathogen but do not harm the human host. By targeting the epitopes and disrupting the functions of these key enzymes, we hope to provide more effective solutions to treat multidrug-resistant TB,” said Professor Gerhard Grüber, the lead Principal Investigator of TOPNet* at NTU’s School of Biological Sciences.
Scientists in EDDC’s High Throughput Screening (HTS) and Medicinal Chemistry teams developed chemical-based inhibitors against these two targets. In one project, EDDC’s HTS team, led by Dr Choong Meng Ling, screened over 115,000 small molecule compounds to identify those that would bind well and was effective in inhibiting Cyt bd. Through a rigorous and iterative process of functional bioassays and compound optimization, a lead series of potent inhibitors were generated.
In a second project, EDDC’s medicinal chemists further optimised a previously discovered inhibitor of F1FO-ATP synthase through repeated cycles of testing and re-design. Likewise, this project led to the development of a lead series of compounds. A patent has been filed for the inhibitors developed for this target, with licensing discussions underway with a pharmaceutical company. This effort is led by NTUitive, NTU’s innovation and enterprise company.
“This was a true partnership where each partner brought complementary expertise to the table. We used our capabilities at EDDC to generate these compounds, which our collaborators at NTU and LKC Medicine then tested in biological assays to determine which worked and which didn’t. In so doing, we were able to develop these novel, potent compounds in a very focused fashion,” said Pearly Ng, Head of Medicinal Chemistry at EDDC.
Prof Grüber agreed, “It has indeed been a fruitful collaboration with EDDC. We worked like a seamless tag-team, matching our capabilities to allow each partner to focus on what each does best. It has been critical to the success of this partnership.”
As other superbugs loom large in our environment, the EDDC and NTU teams are not resting on their laurels. They are currently in discussion to expand their successful collaboration and develop therapies to tackle more superbugs.